The use of CBCT in oral implantology today has most commonly been used for diagnosis and treatment planning. However, little has been documented on the evaluation of peri-implant disease and the long-term success of dental implants. Peri-implant disease is a major post-operative concern, as recent studies have shown a very high prevalence. Therefore, it is imperative that the dental implant clinician have the ability to evaluate accurately the post-operative periimplant condition around implants.
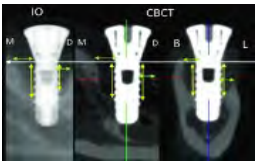
Problem: Intra-Oral Radiographs: In clinical practice today, in the evaluation of dental implants, intraoral radiographs (periapical and bitewings) are the most commonly used. However, these radiographs have significant limitations as they are a two-dimensional representation of a three-dimensional anatomic structure, high degree of geometric distortion and magnification and low spatial resolution. Most importantly, these radiographs do not depict the amount of buccal or lingual bone loss, which is a crucial aspect of evaluating peri-implant health. Numerous studies have shown that intraoral radiographs underestimate the amount of peri-implant bone loss.1 2
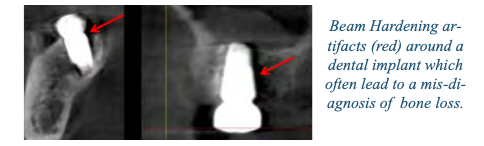
CBCT Images: Cone Bean Computerized Tomography (CBCT), with its inherent 3-dimensional capability, is the ideal radiographic modality to evaluate all aspects of the implant without overlap. However, CBCT images have been depicted as having a degree of artifact inaccuracies. This is mainly a result of the dental implant material absorbing X-rays, which leads to the deterioration of images through artifacts such as beam hardening, scatter, and streaking.
These artifacts have been shown to negatively affect the evaluation of the bony contours around an implant. When an X-ray beam contacts a high-density object (e.g., implant, abutment, prosthesis), lower-energy photons are absorbed more than high-energy photons. This will result in beam hardening, which creates cupping, streaks, and band artifacts. Often, these artifacts result in the misdiagnosis of pathology or bone loss.
Dental Implant Material: The type of dental implant material is very significant with respect to the amount of artifacts present. In comparing titanium alloy and zirconia implants, Sancho-Puchades et. al. showed that zirconia implants produced significantly more artifacts that titanium implants. The amount of photons that are absorbed is directly dependent on the material. Because zirconia has a higher atomic number than titanium, there exists a greater formation of artifacts with this type of material.3
CBCT Linear Measurements: Although CBCT images have been shown to be very accurate for millimeter range measurements, studies have shown a degree of inaccuracy when measuring around implants. Recent research has shown measurements less than 0.5 mm have inherent inaccuracies.4 5 Therefore, absolute linear measurements directly next to implants may be associated with errors with very thin and incipient compromised sites.
In the evaluation of bony defects around implants, CBCT has been shown to be superior to Intra-Oral radiographs.
Conclusion: In the evaluation of bony defects around implants, CBCT has been shown (even with artifacts) to be more accurate than conventional intraoral radiography with respect to the detection of fenestrations, dehiscence’s, and periodontal defects.6 Therefore, what does the future of CBCT in the evaluation of implants hold? The amount of artifact on CBCT images is highly dependent on the type of CBCT unit, protocol settings, and implant material. First, implant clincians may improve accuracy by decreasing the voxel size of the CBCT unit as the voxel size has been shown to be clinically relevant with respect to artifacts. A voxel size of 0.150 mm3 has been shown to be the ideal size to accurately view bony defects.7 As far as future research and development in improving CBCT image quality, the most promising include software modifications such as the metal artifact reduction (MAR) algorithms. These algorithms appear to be the answer in decreasing artifacts and improving linear measurement calculations. 8
1 Christiaens, V., De Bruyn, H., De Vree, H., Lamoral, S., Jacobs, R., & Cosyn, J. (2018). A controlled study on the accuracy and precision of intraoral radiography in assessing interproximal bone defect morphology around teeth and implants. European Journal of Oral Implantology, 11, 361–367.
2 Garcia-Garcia, M., Mir-Mari, J., Benic, G. I., Figueiredo, R., & Valmaseda- Castellon, E. (2016). Accuracy of periapical radiography in assessing bone level in implants affected by peri-implantitis: A cross-sectional study. Journal of Clinical Periodontology, 43, 85–91. https://doi. org/10.1111/jcpe.12491
3 Sancho-Puchades, M., Hämmerle, C. H., & Benic, G. I. (2015). In vitro assessment of artifacts induced by titanium, titanium-zirconium and zirconium dioxide implants in cone-beam computed tomography. Clinical Oral Implants Research, 26, 1222–1228. https:// doi.org/10.1111/clr.12438
4 Gröbe, A., Semmusch, J., Schöllchen, M., Hanken, H., Hahn, M., Eichhorn, W., … Precht, C. (2017). Accuracy of bone measurements in the vicinity of titanium implants in cbct data sets: A comparison of radiological and histological findings in minipigs. BioMed Research International, 2017, 1–9. https://doi.org/10.1155/2017/3848207
5 Pelekos, G., Acharya, A., Tonetti, M. S., & Bornstein, M. M. (2018). Diagnostic performance of cone beam computed tomography in assessing peri-implant bone loss: A systematic review. Clinical Oral Implants Research, 29, 443–464. https://doi.org/10.1111/clr.13143
6 Song, Dandan, et al. “Diagnostic accuracy of CBCT versus intraoral imaging for assessment of peri‐implant bone defects.” BMC Medical Imaging 21.1 (2021): 1-8.
7 Kurt, Mehmet Hakan, et al. “Comparison of the different voxel sizes in the estimation of peri-implant fenestration defects using cone beam computed tomography: an ex vivo study.” International Journal of Implant Dentistry 6.1 (2020): 1-11.
8 Nagarajappa, Anil Kumar, Neha Dwivedi, and Rana Tiwari. “Artifacts: The downturn of CBCT image.” Journal of International Society of Preventive & Community