The posterior maxilla poses a unique challenge to the dental implant clinician as this anatomic area is often deficient in quality and quantity of host bone. Currently, there is an abundance of research studies that have shown very high success rates with grafting and implant placement procedures in the posterior maxilla. However, this anatomic area is not free from complications that may increase patient morbidity and jeopardize the success of implant procedures. [1]
A thorough preoperative examination of the posterior maxilla is required prior to performing implant related procedures in the maxillary sinus area. The implant clinician must have a strong understanding of the potential complications that are commonly associated with the maxillary sinus. Drainage issues have been shown to be one of the most significant etiologic factors which may lead to impaired mucociliary function and sinus disease.
There exists many factors which may lead to post-operative maxillary sinus related issues. The most common is existing sinus pathology which is maybe symptomatic or asymptomatic. Hsiao et. al. concluded that maxillary sinus pathology to be approximately 37% in a dental school patient population study. [2] However, an often-overlooked factor is anatomic variations of the paranasal sinuses. [3] [4] Anatomic variant anatomy is defined as abnormalities or atypical findings within anatomical structures which may or may not interfere with normal function of anatomic area. Studies have shown the paranasal sinuses have a high prevalence rate of variant anatomy which may range from 67% – 85%. [5] Therefore, it is important to diagnosis and determine if variant anatomy within the paranasal sinuses may contribute to post-operative dental implant procedure morbidity.
The Effects of Dental Implant Procedures on Sinus Physiology
The maxillary sinus is the most infected sinus of all the paranasal sinuses in the head and neck region. [6] The physiologic balance of the maxillary sinus has been shown to be easily altered by viruses, bacteria, and foreign bodies. However, when pathology and anatomic variants are not present in the maxillary sinus, implant related procedures usually result in only a transient effect on the sinus physiology.
Timmenga et. al. has shown a temporary clearance impairment that produces only subclinical effects on maxillary sinus physiology after bone grafting procedures in the sinus. After manipulation of the membrane and grafting of the sinus, the pre-surgical sinus physiology most commonly will return to normal in approximately 9 months. [7] However, there are many reports and case studies in the literature describing patients that have developed chronic pathologic conditions such as post-operative chronic rhinosinusitis. In these cases, most commonly sinus pathology or anatomic variants were present and a predisposing factor. [8] [9] Because of the existing pathology or atypical anatomy, maxillary sinus drainage was compromised to increase post-op complications. [10] [11]
Therefore, it is imperative the implant clinician have a strong foundation for the pre-operative evaluation and diagnosis of normal vs. abnormal anatomy that may lead to post-operative complications.
Osteomeatal Complex
The osteomeatal complex is defined as the anatomical area that represents the common pathway for drainage and ventilation of the frontal, anterior ethmoid, and maxillary sinuses. Studies have shown that approximately 90% of chronic maxillary rhinosinusitis cases are caused by anatomic variations within the osteomeatal complex [12] Therefore, the osteomeatal complex must be fully understood and appreciated prior to dental implant procedures in this area. Anatomically, there exists five important structures which comprise the osteomeatal complex: [13]
- Maxillary Ostium: main drainage area of the maxillary sinus
- Infundibulum: pathway or channel that allows drainage from the maxillary sinus to the hiatus semilunaris
- Ethmoid Bulla: an air cell that projects over the hiatus semilunaris
- Uncinate Process: bony, hook-like process that forms the anterior boundary of the hiatus semilunaris [14]
- Hiatus Semilunaris: a groove in the lateral wall of the middle meatus which is the final drainage passage of the maxillary sinus
The function or health of the osteomeatal complex after maxillary sinus implant procedures is dependent on the patency of the maxillary sinus ostium. When the maxillary ostium becomes blocked (non-patent), the normal drainage and ventilation within the paranasal sinuses is compromised leading to active disease processes including.[15]
- Impaired Drainage
- Increase in CO2 Concentration
- Decrease in O2 Concentration
- Impaired Cilia Activity
- Epithelial Dysfunction and Metaplasia
- Decrease in Ventilation
Therefore, it is imperative the implant clinician must ascertain that the maxillary ostium is patent prior to surgery and post-operatively during the healing period.
The Importance of Maxillary Sinus Ostium Patency
The main drainage avenue of the maxillary sinus is via the maxillary ostium. The maxillary ostium is the primary pathway for secretions within the maxillary sinus to clear and drain into the middle meatus. To maintain paranasal health, a physiologic balance between the mucociliary clearance characteristics of the maxillary sinus and osteomeatal complex is crucial.
Anatomically, the maxillary ostium is bounded superiorly by the ethmoid sinuses and inferiorly by the uncinate process. It is located within the superior aspect of the medial wall of the maxillary sinus and in health is approximately 2.4 mm in diameter. [16]
In patients free of sinus disease and lack of anatomic variants, procedures that manipulate the sinus mucosa do not appear to result in sinus disease. This can be easily verified by the low incidence of acute rhinosinusitis after these procedures (<1%). [17] The sinus membrane is known to heal rapidly, however if there is any compromise in the drainage avenues of the osteomeatal complex, healing may be delayed with resultant sinus disease. Timmenga et. al. concluded that the maxillary sinus mucosa is capable of adapting to changes induced by implant related procedures when sinus clearance is not compromised. [18]
Prior to any procedures involving the maxillary sinus proper (e.g. bone grafting, implant placement), the patency of the maxillary ostium must be determined. If the ostium is non-patent, then the mucociliary clearance of the maxillary sinus may be affected which may lead to an increased morbidity with implant-related procedures. Anytime the maxillary sinus proper is compromised (i.e. sinus bump, sinus elevation, implant insertion into sinus) post-operative swelling of the sinus mucosa (Schneiderian Membrane) is an unavoidable sequela. When thickened sinus mucosa is present, a compromised maxillary sinus drainage may result which along with a compromised maxillary ostium diameter. [19] [20]
Radiographic Evaluation:
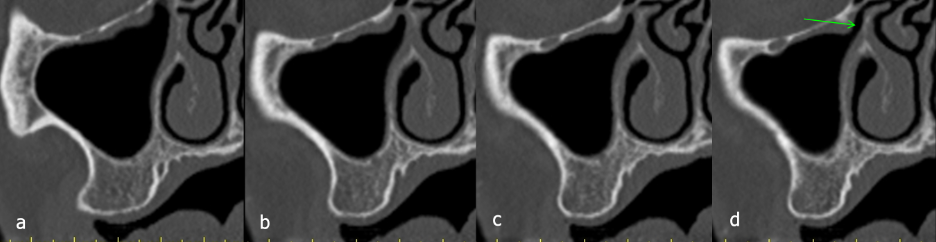
The most common technique to visualize the maxillary ostium is with coronal CBCT images. By scrolling through various coronal images, the opening can be verified by evaluating the medial wall of the maxillary sinus (lateral wall of nasal cavity). (Figure 1)
Figure 1: (a-d) Serial cross-sectional images showing the progression of the patency of the maxillary ostium (red arrows-non-patent), (green-patent).
Anatomic Variations:
Anatomic variants within the paranasal sinuses may interfere with the normal drainage and ventilation processes of the maxillary sinus via ostium blockage. When this occurs, the risk of sinus mucosal disease increases significantly. Studies have shown the larger the size of the anatomic variant, the increased possibility of paranasal sinus mucosal alterations. [21] Therefore, it is imperative the implant clinician be able to diagnosis and detect the atypical and anatomic variants on computed tomographic images.
The most common anatomic variants in the paranasal sinuses leading to ostium non-patency include a concha bullosa, paradoxical middle turbinate, deviated septum, and haller cells.
- Concha Bullosa
The middle turbinate (nasal concha) plays a significant role in proper drainage function of the maxillary sinus. Normally the middle turbinate is a thin, bony structure, however, it can be aerated, which is termed a concha bullosa. This pneumatization of the middle turbinate may be unilateral or bilateral, and it has been shown to have a prevalence rate of up to 53.6% of the population. [22]
Radiographic Evaluation
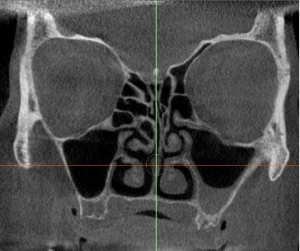
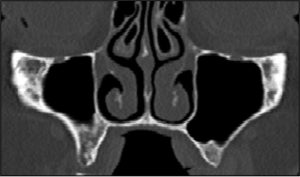
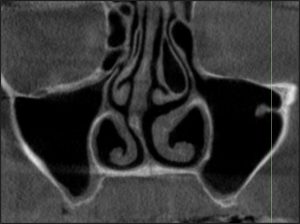
A concha bullosa variant in the middle turbinate may be easily identified on a CT/CBCT coronal image depicting a radiolucent air space in the center of the middle meatus and surrounded by an ovoid bony rim. (Figure 2)
Clinical Significance
When a concha bullosa is present, there exists the potential for narrowing or occlusion of the maxillary sinus ostium. The larger the concha bullosa, the more likely the probability of compromising the drainage of the maxillary sinus. When enlarged, pressure against the uncinate process may occur, decreasing the infundibulum drainage, and thus affecting the physiology of the maxillary sinus. When this occurs, the mucociliary function of the sinus is compromised. Thus, the implant clinician must ascertain the probability of post-operative complications with respect to the size of the concha bullosa. When concha bullosa’s are present that may compromise the drainage of the maxillary sinus, or the patient has a history of drainage issues, an Otolaryngologist consultation is warranted for evaluation and possible surgical correction.
Figure 2: (a) Unilateral Concha Bullosa, (b) Bilateral Concha Bullosa.
- Paradoxical Middle Turbinate
A paradoxical middle turbinate is an anatomic variant of the middle turbinate that is characterized by a laterally directed convexity. Normally, the convexity of the paradoxical middle turbinate is directed medially toward the nasal septum. Because a paradoxical middle turbinate is “backwards”, blockage of the infundibulum may occur along with the maxillary ostium being non-patent. The prevalence of paradoxical middle turbinates is approximately 34%. [23]
Radiographic Evaluation A paradoxical middle turbinate is most commonly evaluated on a coronal CT/CBCT scan image. In addition, serial cross-sectional images will readily depict the middle turbinate convexity directed laterally.
(Figure 3)
Clinical Significance When present, a paradoxical middle turbinate may lead to obstruction of the maxillary ostium with possible drainage issues within the sinus. If radiographic evidence shows significant occlusion of the osteomeatal complex from a pardoxical middle turbinate, prior to dental implant procedures, a Otolaryngologist consultation is recommended for evaluation and possible surgical correction.
Figure 3: Paradoxical Middle Turbinate
- Deviated Septum
One of the most common anatomic variants in the paranasal sinuses is a deviated septum, which may be congenital or traumatic in origin. This occurs when the nasal septum is displaced laterally toward one side of the nasal cavity. The nasal septum is an osseocartilaginous wall that divides the right and left side of the nasal cavity. At the junction of the nasal cartilage with the vomer bone, an acute angulation occurs which results in a deviation of the nasal septum. [24]
Studies have shown a prevalence rate of up to 70%, which increases the possibility of ostiomeatal complex blockage. [25]
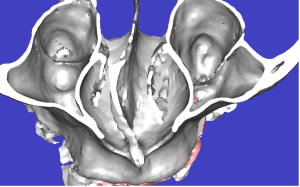
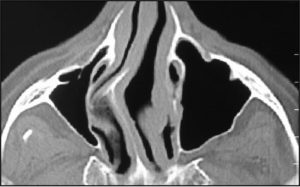
Radiographic Evaluation A deviated septum is most easily seen on coronal and axial images. In addition, CBCT 3D images allow for direct visualization to the extent and angulation of the septal deviation. (Figure 4)
Clinical Significance When the deviation is severe, the airflow through the nasal cavity is compromised, most commonly manifesting as nasal congestion. Patients with deviated septum’s are predisposed to sinus clearance issues, which increase morbidity of bone grafting and implant placement procedures in the maxillary posterior area on the side of deviation. In most cases the contralateral side will have normal mucociliary clearance. When significant blockage is evident, the patient should be referred to an Otolaryngologist for consultation.
Figure 4: Deviated Septum (a) 3D Image, (b) Axial CBCT Image
- Haller Cell
Haller cells are anatomic variants within the ethmoid air cells and considered an anterior extension of the ethmoid sinus into the superior aspect of the maxillary sinus. Haller cells have been shown to have a prevalence ranging from 20% – 43%. [26] [27]
Because of the positioning of Haller Cells, they may cause compression and narrowing of the infundibulum which may lead to inflammation and infection. This anatomic variant may decrease the size of the ostium/osteomeatal complex (OMC) which may predispose dental implant patients to ipsilateral maxillary sinus disease and obstruction. [28]
Radiographic Evaluation
Haller cells can be distinguished radiographically by a radiolucent air-filled cavity located medially on the orbital floor, inferior to the ethmoid bulla (large ethmoidal cell). This anatomic variant may vary greatly in size and shape, and most commonly seen on coronal CBCT images. [29]
Clinical Significance
Haller cells may predispose patients to sinus disease by causing obstruction of the maxillary sinus ostium which may lead to blockage of sinus drainage and result in post-operative sinus complications. Larger Haller cells are associated with maxillary sinus disease and should be evaluated for possible post-operative implant complications and referral to an Otolaryngologist for evaluation. [30] [31]
Figure 5: Haller Cell (a-b)

Conclusion
Placement of implants and bone grafting in the maxillary posterior is a reliable and predictable procedure under healthy conditions. However, the dental implant clinician must adhere to strict protocols to prevent complications and increased morbidity. A pre-operative CBCT examination should always be completed and evaluated for predisposing conditions which may lead to post-surgical paranasal sinus complications. Studies have shown that grafting and implant placement into the maxillary sinus without radiographic sign of disease or anatomic variants does not predispose patients to sinusitis related complications. [32]
However, anatomic variants may compromise and disturb the drainage avenues and ventilation aspects of the maxillary sinus. Having an understanding of the direct influence of anatomic variants on the osteomeatal complex, clinicians should be conscious of the impaired maxillary sinus conditions which may result and the alteration in the normal physiology of the maxillary sinus.
Therefore , evaluation of the maxillary sinus ostium via serial cone beam computerized tomography (CBCT) must be ascertained prior to surgery to minimize potential post-operative complications. In addition, the patency of the maxillary ostium must be maintained throughout the healing period. If not, the mucociliary action of the maxillary sinus will be compromised. In cases of compromised drainage, referral to an Otolaryngologist is warranted for evaluation and possible surgical correction prior to implant related procedures.
[1] Zijderveld, Steven A., et al. “Anatomical and surgical findings and complications in 100 consecutive maxillary sinus floor elevation procedures.” Journal of Oral and Maxillofacial Surgery 66.7 (2008): 1426-1438.
[2] Hsiao, Y. J., Yang, J., Resnik, R. R., & Suzuki, J. B. (2019). Prevalence of maxillary sinus pathology based on cone-beam computed tomography evaluation of multiethnicity dental school population. Implant dentistry, 28(4), 356-366
[3] Valentini P, Hadchiti W, Abensur D. Maxillary sinus grafting: A proposal for avoidance of postoperative complications. Ann Oral Maxillofac Sur 2013;1:23-28.
[4] Timmenga NM, Raghoebar GM, van Weissenbruch R, Vissink A. Maxillary sinus floor elevation surgery. A clinical, radiographic and endoscopic evaluation. Clin Oral Implants Res 2003;14:322-8.
[5] Pérez-Piñas, Sabaté J, Carmona A, Catalina-Herrera CJ, Jiménez-Castellanos J. Anatomical variations in the human paranasal sinus region studied by CT. J Anat 2000;197 (Pt 2):221-7.
[6] American Family Physician. “Acute Sinusitis”. July 2016. Accessed 18 July 2018.
[7] Timmenga, Nicolaas M., et al. “Maxillary sinus function after sinus lifts for the insertion of dental implants.” Journal of Oral and Maxillofacial Surgery 55.9 (1997): 936-939.
[8] Valentini P, Maxillary sinus grafting: A proposal for avoidance of postoperative complications. Annals of Oral & Maxillofacial Surgery 2013 Aug 01;1(3):23.
[9] Barone, A., Santini, S., (2006) A clinical study of the outcomes and complications associated with maxillary sinus augmentation. Int J Oral & Maxill Implants 21:81–85.
[10] Peleg, M., (1999) Radiological findings of the post sinus lift maxillary sinus: a computerized tomography follow up. Journal of Periodontology 70: 1264–1273.
[11] Doud Galli, S.K., (2001) Chronic sinusitis complicating sinus lift surgery.American Journal of Rhinology 15: 181–186.
[12] Utara, Sumatra, and RS H. Adam Malik. “The clinical features of ostiomeatal complex in chronic maxillary sinusitis by nasoendoscopic examination.” (2006).
[13] Laine F & Smoker W. The Ostiomeatal Unit and Endoscopic Surgery: Anatomy, Variations, and Imaging Findings in Inflammatory Diseases. AJR Am J Roentgenol. 1992;159(4):849-57
[14] Laine F & Smoker W. The Ostiomeatal Unit and Endoscopic Surgery: Anatomy, Variations, and Imaging Findings in Inflammatory Diseases. AJR Am J Roentgenol. 1992;159(4):849-57.
[15] Mantovani M. Otolaryngological contraindications in augmentation of the maxillary sinus. In: Testori T, Del Fabbro M, Weinstein R, Wallace S, editors. Maxillary Sinus Surgery and Alternatives. 1st ed. Chicago: Quintessence; 2009. p. 42-52.
[16] Aust, R., and B. Drettner. “The functional size of the human maxillary ostium in vivo.” Acta oto-laryngologica 78.1-6 (1974): 432-435.
[17] Bhattacharyya N. Bilateral chronic maxillary sinusitis after the sinus-lift procedure. Am J Otolaryngol. 1999;20:133–135.
[18] Timmenga, Nicolaas M., et al. “Effects of maxillary sinus floor elevation surgery on maxillary sinus physiology.” European journal of oral sciences 111.3 (2003): 189-197.
[19] Aust R, Stiema P, Brettner B: Basic experimental studies of ostial patency and local metabolic environment of the maxillary sinus. Acta Otolaryngol 515:7, 1994
[20] Drettner B: The permeability of the maxillary ostium. Acta Otolaryngol 60:500, 1975.
[21] Liu X, Han D, Zhou B. Relationship between anatomic variants of nasal sinus and chronic sinusitis. Zhonghua Er Bi Yan Hou Ke Za Zhi. 1998;33:149–152.
[22] Stammberger H, Wolf G. Headaches and sinus disease: The endoscopic approach. Ann Otol Rhinol Laryngol Suppl 1988;134:3-23.
[23] El-Anwar, Mohammad Waheed, et al. “Radiological middle turbinate variations and their relation to nasal septum deviation in asymptomatic adult.” Egyptian Journal of Radiology and Nuclear Medicine 51.1 (2020): 1-5.
[24] Lee, Jang Won, et al. “Correlations between anatomic variations of maxillary sinus ostium and postoperative complication after sinus lifting.” Journal of the Korean Association of Oral and Maxillofacial Surgeons 42.5 (2016): 278-283.
[25] Robinson, Jennifer (December 11, 2016). “What Is a Deviated Septum?”. WebMD.
[26] Yousem DM. Imaging of sinonasal inflammatory disease. Radiology. 1993;188 (2): 303-14.
[27] Pekiner FN, Borahan MO, Dumlu A, Ozbyrak S. Infraorbital ethmoid (Haller) cells: a cone beam Computed tomographic study. Oral Radiol 2014:30; 219- 225.
[28] Rice, Dale H., and Steven D. Schaefer. Endoscopic Paranasal Sinus Surgery. Lippincott Williams & Wilkins, 2004.
[29] Kamdi, Pallavi, et al. “Evaluation of haller cell on CBCT and its association with maxillary sinus pathologies.” Journal of Indian Academy of Oral Medicine and Radiology 30.1 (2018): 41.
[30] Stackpole SA, Edelstein DR. The anatomic relevance of the Haller cell in sinusitis. Am J Rhinol. 1997;11(3):219- 23.
[31] Shrikrishna BH, Jyothi AC, Sanjay G, Samson SG. prevalence of anatomic variations in chronic rhinosinusitis. J Evol Med Dent Sci 2013;2(11):1609- 1617.
[32] Timmenga, Nicolaas M., et al. “Maxillary sinus function after sinus lifts for the insertion of dental implants.” Journal of Oral and Maxillofacial Surgery 55.9 (1997): 936-939.