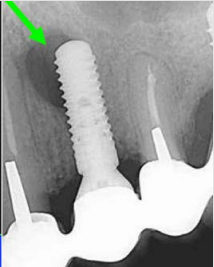
Following implant placement and recall examinations, case reports have shown the genesis of periapical lesions (radiolucency) at the implant apex, which may suggest a possible precursor to failure of the endosseous implant. In most cases, a periapical lesion is present while the coronal portion of the implant remains free of bone loss. These periapical lesions have been termed apical peri-implantitis or retrograde periimplantitis. The prevalence of these lesions has been shown to be less than 1%, however, when the implant site is near an adjacent root-canaled tooth, the prevalence has been shown to increase to approximately 8%. Because of the multifactorial etiology of periapical lesions around dental implants, there is no accepted general consensus on the treatment. The treatment regimen is defined by subjective and objective symptoms.
Asymptomatic. A clinically asymptomatic periapical radiolucency is considered to be inactive when radiographically there exists evidence of bone destruction with no clinical symptoms. This may result from placing an implant into a site in which the osteotomy was prepared deeper than the implant length, resulting in an apical space. Also, when implants are placed adjacent to a tooth with an apical scar or endodontic pathology, this may result in a radiolucency. Usually, treatment will include close observation and if bony changes do occur, surgical intervention is recommended.
Symptomatic. A clinically symptomatic lesion is most commonly caused by bacterial contamination during implant placement. This may occur when an implant is placed into a preexisting area with bacteria (existing infection, cyst, granuloma, or abscess). When lesions are initiated at the apex, they may spread coronally or facially. Treatment for a symptomatic lesion involves exposure, debridement, surface decontamination, allograft + membrane.