With full-arch implant prostheses, adequate hygiene practices provide for decreased complications and increased longevity of the implants and prosthesis. If the prosthesis is inadequately cleaned, the patient will be predisposed to potential peri-implant complications. An often question asked by clinicians is “Should the prosthesis be removed, cleaned, and re-inserted on routine maintenance appointments”?
Unfortunately, in the dental implant literature, there exist no accepted scientific evidence or guidelines for maintenance of full-arch prostheses.[1] Basically, the ideal technique and protocol to maintain full arch prostheses and supporting tissues are controversial and poorly defined. Therefore, there exist many schools of thoughts on whether it is advantageous or problematic for the continuous removal of full arch prostheses.
Why Are Full-Arch Prostheses Predisposed to Complications?
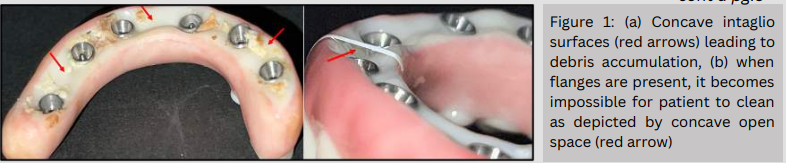
Because of the inherent design of full-arch fixed prostheses, biofilm accumulation and restricted access for hygiene are common problems. The prosthesis design is strongly dictated by the position of the implants and the teeth, which is often non-ideal because of the bone resorption process. The most common design flaw is the intaglio surface being concave (i.e., ideally convex), which limits access to hygiene procedures. Therefore, biofilm and other debris will accumulate which results in poor tissue health and the development of peri-implant disease. (Figure 1)
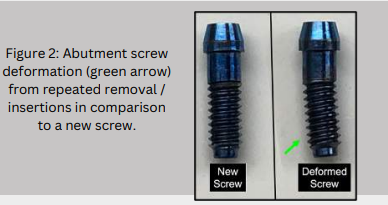
The main documented complication of prosthesis removal is the potential damage of the abutment screws after removal of the prosthesis. Because of the mechanical forces that are applied to the screw (preload with resulting clamping force), the mechanical properties of the abutment screws are irreversibly modified. When an abutment screw is tightened (i.e., 30 N/cm with a torque wrench), a force is generated between the abutment and implant. The abutment and implant are held together by a “clamping force”, which results from the applied rotational torque force called “preload”. The abutment screw when torqued will become an “elongated spring”, which results in tension on the screw threads. There is a resultant elastic recovery of the thread, which creates a force (clamping force) that results in friction between the abutment and implant. After the initial torque, approximately 2 – 10% of the initial preload is lost, which is a phenomenon termed “embedment relaxation” or “settling effect”. [2] This loss of preload is counteracted by re-torquing the screws to the initial torque 5-10 minutes after the first torque. Therefore, the entire torquing process will result in changes to the abutment screw physical properties. Various clinical studies have evaluated the ramifications of the removal and re-insertion of abutment screws. Rangert et al., concluded that removal and tightening of abutment screws led to altered interface stability, mainly from alteration of the mechanical and physical properties. This may result in screw loosening or screw fracture. [3] Butkevica et al. reported that repeated tightening and loosening of abutment screws will result in torque‐level changes. Their studies concluded that ideally the number of tightening/loosening cycles should be limited. [4] Arshad et al. evaluated the effect of repeated screw joint closing and opening cycles and cyclic loading on abutment screw removal torque and screw thread morphology using scanning electron microscopy (SEM). All groups in the study exhibited reduced removal torque values in comparison to insertion torque values in each cycle. [5] In summary, re-insertion of the prosthesis with the same screws will increase the potential for screw loosening and fracture. Therefore, ideally screws should be replaced after each reinsertion, however this is costly and, in most cases, impractical. Unfortunately, it is impossible to generalize for all clinical situations and various types of screws, as manufacturers screws differ in initial torque, screw material, screw geometry, number and pitch of screw threads and application of a second torque. (Figure 2)
So, what are the advantages and disadvantages of removing the prosthesis for maintenance appointments?
Advantages –
- Access to the implant and abutments for hygiene
- Ease of cleaning and polishing the prosthesis
- Modification of the prosthesis if indicated
Disadvantages –
- Time-consuming
- Abutment screw deformation
- Possible increased screw loosening/fracture
- Possible need to replace abutment screws
- Increased stress to the implant from removal/insertion of screws
What is the position of the American College of Prosthodontics (ACP)?
In 2016, The American College of Prosthodontics’ published a position paper stating that full-arch implant prostheses should not be removed at routine hygiene visits.[1] However, it is their position if the prosthesis does not allow for adequate cleaning or signs and symptoms are consistent with peri-implant disease, then the prosthesis should be removed.
Summary:
- There exists no clear scientific evidence on the professional technique and protocols to manage full-arch fixed implant prostheses.
- It is imperative the clinician and patient implement a long-term maintenance program that will access patient compliance and facilitate early detection of potential complications.
- The patient must understand they have a responsibility in maintaining ideal hygiene, however it is the clinician’s responsibility to provide a prosthesis that is easily cleansable.
- Ideally, the full-arch implant prostheses should be designed to allow for access and proper cleansability (convex intaglio surface)
- The prosthesis removal, cleaning, and reinsertion is the easiest technique to remove debris from the prosthesis, however it may lead to complications.
- The main long-term disadvantage of continued prosthesis removal is the irreversible alteration of the abutment screws which may lead to screw loosening/fracture.
Conclusion:
In most clinical situations, the prothesis should not be removed for routine maintenance. However, if any of the following are present, removal is recommended to properly clean and modify the prosthesis if necessary;
- There exists debris accumulation that cannot be removed via standard hygiene practices.
- The prosthesis design has inherent physical obstacles that prevent proper hygiene
- There is active peri-implant disease (peri-mucositis or peri-implantitis)
Generalized Guidelines If Prosthesis IS Removed
* If the prosthesis requires removal (as per the criteria above), the implants and abutments should be cleaned via conventional hygiene methods. The prosthesis should be mechanically cleaned to remove biofilm and any debris build-up. The prosthesis may be placed in an ultrasonic bath cleaner (with tartar and stain remover) and then highly polished to obtain a surface which will minimize biofilm accumulation.
* There exist no accepted guidelines on the replacement of abutment screws after removal. Many variables exist, such as screw diameter, material number of threads, number of implants which need to be considered when replacing screws. Therefore, the clinician should evaluate the need to replace screws on a case-by-case basis depending on the above-mentioned factors.
* Care should be exercised in immersing the prosthesis in disinfected proprietary solutions as they may have an adverse effect on the surface properties of the prosthesis. Therefore, only use solutions that are approved via the manufacturer’s specific materials instructions. Generalized Guidelines If Prosthesis IS NOT Removed The regular hygiene practices on a prosthesis should include titanium scalers, ultrasonics, or rubber cup with a fine grit polishing paste. Studies have shown that glycine powder air polishing is the most effective alternative to manual and mechanical instrumentation. [6]
[1.] Piermatti, J., P. Barndt, and G. Thalji. “Maintenance of Full-Arch Implant Restorations.” Barndt P, editor (2016).
[2.] Shingley JE, Mischke CR, Standard handbook of machine design, 1st ed. New York: McGraw Hill 1986; 23-6.
[3.] Rangert, B. O., et al. “Bending overload and implant fracture: a retrospective clinical analysis.” International Journal of Oral and Maxillofacial Implants 10.3 (1995).
[4.] Butkevica, A., Nathanson, D., Pober, R., and Starting, H. (2018). Measurements of repeated tightening and loosening torque of seven different implant/abutment connection designs and their modifications: an in vitro study. The Journal of Prosthodontics 27 (2): 153–161.
[5.] Arshad, M., Mahgoli, H., and Pavaminia, L. (2018). Effect of repeated screw joint closing and opening cycles and cyclic loading on abutment screw removal torque and screw thread morphology: scanning electron microscopy evaluation. The International Journal of Oral and Maxillofacial Implants 33 (1): 31–40.
[6.] Menini, Maria, et al. “Efficacy of air-polishing devices without removal of implant-supported full-arch prostheses.” International Journal of Oral Implantology 14.4 (2021).